DOX|RTE Offers Quick Insurance Benefits Verification
KSB Dental is continuously working to develop innovations for our DOX|Pedo Technology Suite™, providing greater functionality to every practice. From advancements in practice-to-parent digital communication, charting documentation, and management solutions, we are always looking ahead, attempting to anticipate the changing needs of pediatric dentists. However, we would like to take a moment to look at one of our existing DOX features that you may not know much about.
DOX’s Real Time Eligibility (RTE) allows a member of the front desk staff to electronically verify any patient’s insurance coverage and, within seconds, receive detailed benefit information. Instead of needing a designated employee to spend hours, if not days, on the phone or internet, looking up every insurance company to find a patient’s insurance benefits, RTE handles the requests for multiple patients with ease.
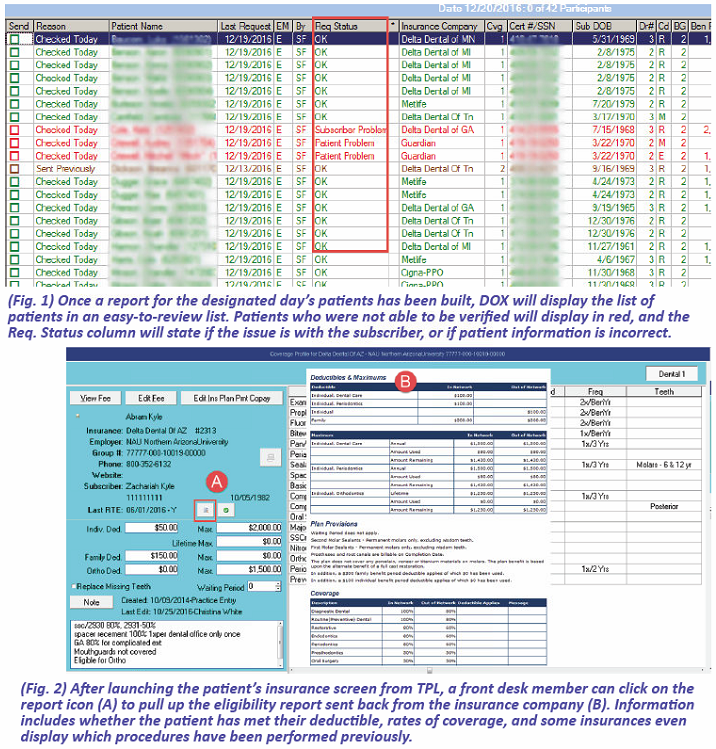
Using KSB’s RTE tool, your staff is able to generate a list of patients coming in on a designated day of operation. Once eligibility has been checked, the report you see in (Fig. 1) allows your staff to quickly view those patients that have eligibility concerns (red), versus those with no concerns (green). Even those patients whose insurances do not participate in receiving an electronic RTE request can be seen on this list, and their eligibility updated once a manual request has been completed.
This color-coded information easily allows the front desk team members to review these patients and be proactive in obtaining any necessary information before the appointment, instead of when the patient is at the check-in desk. Additionally, staff members can quickly check to see if any subscribers are missing their “Cert/SSN” information (critical knowledge for claims to be paid). Using RTE, all these issues can be corrected before an insurance claim is sent out, saving the practice valuable time.
When a team member runs the RTE tool for an entire day’s list of patients, the eligibility request goes out of DOX to the clearing house, then to the insurance company, and right back to DOX within approximately 5 seconds per patient. Once an inquiry comes back from the clearing house, users are able to go to the patient’s insurance information and review a report from the insurance company that lists an overview of their benefits. (Fig. 2)
This information is specific to the insurance company, and is not a one-size-report-fits-all display. Some insurances will even provide when the last date of service was on a few key procedure codes (which is very helpful especially if your office was not the last office to see the patient) and not only how much their deductible and maximums are but how much they have used and how much they have remaining, all conveniently displayed on one screen. The information that is received back can assist in making sure the Coverage Profile information in DOX (which does have to be manually edited) is up to date so that future insurance estimating is as accurate as possible.
Office staff also have the ability to inquire about a single patient. After entering a new patient’s insurance information, they can quickly check the patient’s eligibility to see if the provided information is accurate. Or, if the office needs to add an emergency patient to the TPL, their information can be accessed before the patient even arrives.
Because all previous reports and inquiries are automatically saved for each patient in DOX, on more than one occasion, offices have been able to successfully show proof of eligibility for a patient’s denied claim by sending the provider a print out of the RTE eligibility report with their claim form.